Lecanemab prefers to bind to a certain size of toxic protein found in people with early-stage Alzheimer’s, new research led by Prof Sir David Klenerman (UK DRI at Cambridge) reveals.
Amyloid beta builds up in aggregates in the brains of people affected by Alzheimer’s. Several drugs targeting the protein have been tested in trials over recent years. These drugs are antibodies that bind to the amyloid beta and facilitate its clearance from the brain, but exactly how this occurs is not yet known.
Using new highly sensitive methods, scientists have detected and visualised amyloid beta protein bound to anti-amyloid drugs in the lab. They found that lecanemab performed best in binding to small oligomeric forms of the amyloid protein, suggesting a working model for treating people in the earlier stages of Alzheimer’s. This suggests that it is best used as early as possible in the disease progression.
The new study, led by a group of researchers with diverse scientific backgrounds, including neuroscientists and chemists from the UK DRI at Cambridge, the UK DRI at UCL, and the VIB-KU Leuven Center for Brain & Disease Research, reveals insight into how four different anti-amyloid drugs interact with amyloid beta protein.
Scientists say the research, published today in the journal Alzheimer’s & Dementia and funded by the UK DRI, explains why the different treatments have had varying levels of success in clinical trials.
Until now, we haven’t really understood exactly how anti-amyloid drugs work, or why some have been more successful than others in testing and clinical trials. With this study, we have been able to start to explain the differences we see when people are treated with these different Alzheimer’s drugs.
Group Leader
In the study, scientists compared four different anti-amyloid drugs: lecanemab, donanemab, aducanumab and gantenerumab. They generated model protein aggregates in the lab, and also tested real aggregates taken from the brains of people who had died with Alzheimer’s.
Aducanumab was first approved by the US Food and Drug Administration (FDA) in 2021, but was discontinued in 2024. Lecanemab and donanemab were approved by the UK’s safety regulator the MHRA in 2024, but are not currently available on the NHS, amid discussion about their cost-effectiveness. In trials, both drugs were reported to slow cognitive decline by around 30%. Testing of gantenerumab was halted in 2022 after it showed no clinical benefit in phase 3 trials. It is now being optimised and rebranded as trontinemab.
Using a new technique pioneered at the UK DRI at Cambridge, the scientists were able to visualise the size of protein aggregate each drug preferred to bind to, and how strongly each drug binds to aggregates. The highly sensitive technique allowed the researchers to detect different sizes of soluble aggregate – from larger clumps of protein, down to very small aggregates.
In Alzheimer’s, a misfolded, sticky form of amyloid beta protein first groups together into small, soluble clumps called oligomers. Oligomers group together in turn to form fibrils, which then give rise to insoluble amyloid plaques. Scientists don’t yet know which form of amyloid is most damaging to cells, but there is evidence to suggest the smaller, soluble oligomers may be most toxic.
The research team found that lecanemab binds strongly to a subset of small soluble aggregates that form early on in disease. They also found that lecanemab could bind at more sites per aggregate, allowing the drug to more effectively coat the toxic protein, making it more likely to be cleared.
Whereas aducanumab and gantenerumab bind with a lower affinity to larger aggregates that form later on in the disease progression. Their results for donanemab showed no binding to the soluble aggregates, suggesting that it preferentially binds to larger insoluble aggregates known as ‘plaques’, which form in the spaces between nerve cells. Further studies are needed to understand the impact of the drugs against insoluble aggregates.
Moving forward, the researchers hope their technique can be harnessed to test new and emerging therapies before they are rolled out into human trials, and offer key insight into how drugs work.
Co-first author Emre Fertan, a PhD student at the UK Dementia Research Institute at the University of Cambridge, said:
“In this study, we analysed how four different anti-amyloid drugs interact with the toxic amyloid beta protein that builds up in the brain in Alzheimer’s disease. We were interested in finding out more about the therapeutic effects of these drugs, by studying which type of aggregates they were targeting.
We found that, of the four drugs, lecanemab was the best at binding to small, soluble aggregates – the kind found in the brains of people with early-stage Alzheimer’s disease. From this, we can conclude that lecanemab is most effective when used at the earliest possible stage of disease.”
Co-first author Jeff Lam, a PhD student at the UK Dementia Research Institute at the University of Cambridge, said:
“With this research, we have shown that aducanumab and gantenerumab bind less strongly than lecanemab and prefer to bind to larger aggregates which form later in Alzheimer’s disease. We also found that lecanemab can bind at more sites per aggregate than aducanumab and gantenerumab, allowing the drug to more effectively coat aggregates.
Due to the blood-brain barrier, there is a low concentration of these therapeutics in the brain, so having more high-affinity binding sites significantly increases the chances of effectively eliminating aggregates.”
Study co-leader Prof Sir David Klenerman, Group Leader at the UK Dementia Research Institute at the University of Cambridge, said:
“Until now, we haven’t really understood exactly how anti-amyloid drugs work, or why some have been more successful than others in testing and clinical trials. With this study, we have been able to start to explain the differences we see when people are treated with these different Alzheimer’s drugs.
In future, we hope there will be a wider application for this technique, in testing new and emerging drugs before they enter clinical trials. If we understand more about the therapeutic effect of these treatments at the pre-clinical stage, we may be able to optimise trial design and obtain better results.”
Study co-leader Prof Bart De Strooper, Group Leader at the UK Dementia Research Institute at UCL and VIB-KU Leuven Center for Brain & Disease Research, said:
“These are very interesting observations. Additional work in my laboratory indicates that lecanemab binds also very well to amyloid plaques and that this is crucial for amyloid plaque removal. At that level both lecanemab and donanemab act very similarly. Further work is needed to understand what is most important: binding oligomeric structures or binding amyloid plaques. This is crucial to understand the benefits of the two available amyloid lowering drugs.”
Reference: Fertan E, Lam JYL, Albertini G, et al. Lecanemab preferentially binds to smaller aggregates present at early Alzheimer's disease. Alzheimer's Dement. 2025; 21:e70086. https://doi.org/10.1002/alz.70086
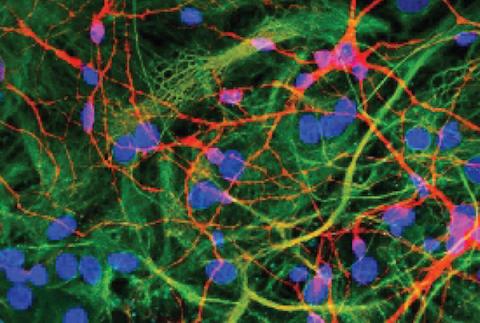
Banner image: Super-resolution microscopy makes it possible to study protein aggregates in high detail. This work shows that Lecanemab preferentially binds to small aggregates, while Aducanumab and Gantenerumab preferentially bind to large aggregates. Credit: Jeff Lam and Emre Fertan.