A new study led by Dr Alexi Nott (UK DRI at Imperial) highlights the role of different brain cell types in genetic risk for neurodegenerative conditions. The research, published in Neuron, reveals potential therapeutic targets for Alzheimer’s.
What was the challenge?
Cerebral small vessel disease is a condition where the brain's tiny blood vessels become narrowed, blocked, or damaged, leading to reduced blood flow. Although 80% of people with Alzheimer’s have some degree of small vessel disease, the conditions appear to have distinct genetic risk factors, and the common molecular mechanisms for their association are not well understood.
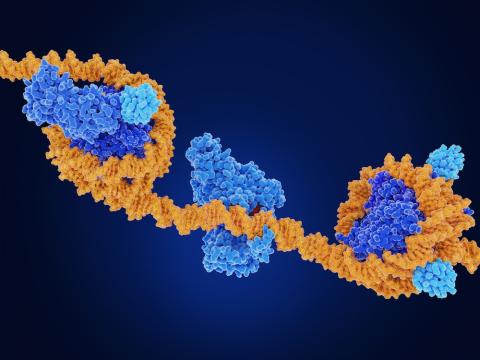
Around 98% of human DNA is non-coding, meaning it does not store instructions for making proteins. Many of the risk variants for both Alzheimer’s and small vessel disease are found outside of genes, in regions of non-coding DNA known as regulatory elements. These regulatory elements include enhancers, which can dial up the expression of different genes. Enhancers are often far away from the genes themselves, so DNA has to bend and fold to link an enhancer to a target gene.
In this study, the team aimed to understand the impact of these regulatory elements in Alzheimer’s and small vessel disease.
There is a major class of non-coding gene regulatory regions called enhancers, and they act like switches to turn genes on and off. These enhancers tend to be very cell type specific, so they're great for informing which cell types might be impacted by disease.
Group Leader
What did the team do and what did they find?
To examine the effects of the non-coding risk variants, Kevin Ziegler and Aydan Askarova from the Nott Lab worked on enhancers in six different brain cell types. These included rare and understudied cell types such as vascular brain endothelial cells and mural cells. They also looked at astrocytes, which act as support cells in the brain, and microglia, the brain’s resident immune cells.
The researchers found Alzheimer’s genetic risk variants primarily overlapped with enhancer regions in microglia. Enhancers in brain endothelial cells, mural cells, and astrocytes more often overlapped with risk variants for small vessel disease.
Kevin and Aydan then looked at how the DNA is folded in these cell types to tie the enhancers to target genes, to see which genes were impacted by the risk variants. This allowed them to compile a list of risk genes for Alzheimer’s and small vessel disease. The group found that the risk genes for small vessel disease were not the same as for Alzheimer’s, suggesting that immune and vascular cells are affected in different ways.
What is the impact?
This work gives new understanding of the role of vascular cell types in genetic risk for Alzheimer’s and cerebral small vessel disease, and new insight into how risk factors can be inherited. There is little epigenetic data on vascular cell types in individuals with dementia, and the Nott lab plan to research these cells further, with support from the Alzheimer’s Association.
Dr Nott added:
“With this new understanding of how vascular cell types affect risk for Alzheimer’s, we are hoping for better-informed prioritisation of drugs and the design of new drugs for the treatment of dementia.”
The team also hope that their discoveries will be able to guide therapies for Alzheimer’s, working in collaboration with the Chandran Lab in Edinburgh. As part of this study, they cross-referenced their findings with the LINCS Connectivity Map, a database which shows the impact of different therapeutics on gene expression. In doing so, they have identified two drugs which appear to induce gene expression changes that counteract the effect of Alzheimer’s.
In upcoming research, the Nott Lab will focus on the immune system, with support from the Vivensa Foundation. They will be looking at how genetic risk in microglia increases as we age, including early in life, and which proteins drive the change.
Alzforum coverage