New research led by Dr Maura Malpetti and Noah Shapiro (UK DRI at Cambridge) reveals signs of brain shrinkage, inflammation and blood markers for nerve damage can improve prediction of disease progression in progressive supranuclear palsy. The study, published in Brain Communications, could help scientists design more efficient clinical trials for the condition.
What was the challenge?
Progressive supranuclear palsy (PSP) is a brain disease characterised by the build-up of toxic tau protein, along with cell loss and brain shrinkage, and inflammation in brain regions that control movement, cognition and behaviour. This study looked at whether certain brain scans and blood tests could help predict clinical progression in people with PSP.
What did the team do and what did they find?
In this study, the team followed 59 people with PSP, using MRI scans to measure brain shrinkage. A sub-group also had a PET scan to measure brain inflammation, plus a blood test for a nerve damage marker called neurofilament light chain (NfL). The researchers compared these measures with how long people survived after their first scan, as an index of clinical progression.
The team found that people with more shrinkage in deep brain areas (subcortical atrophy) tended to have shorter survival, making this a strong marker that could be used in large clinical trials. In the PET and blood test sub-group, higher levels of inflammation in related brain regions and higher blood NfL levels were also linked to shorter survival, while standard clinical rating scores were not good predictors on their own.
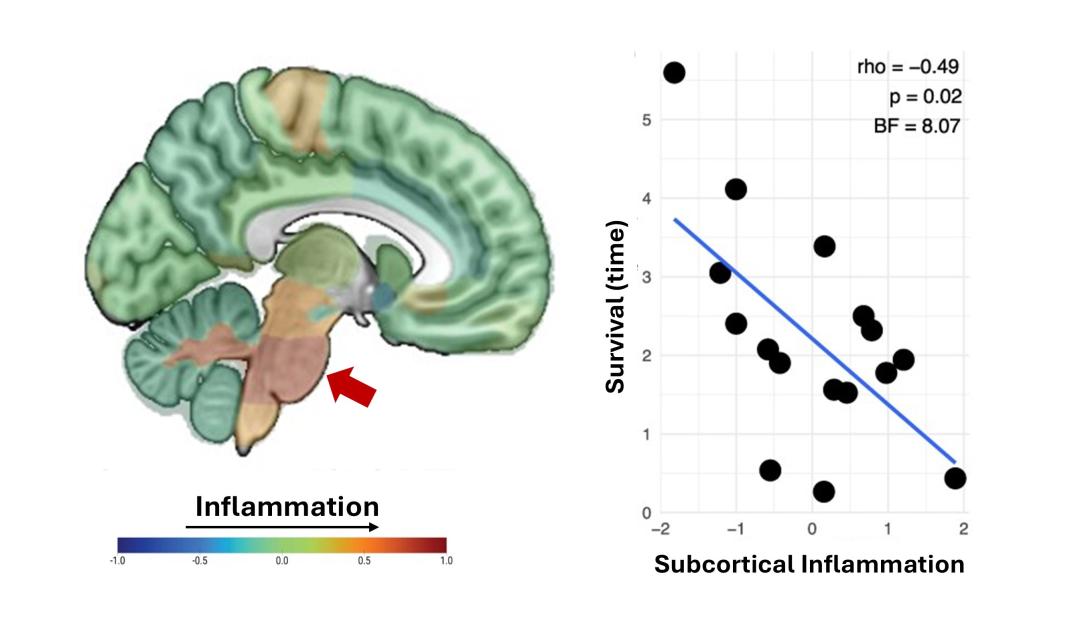
Higher levels of inflammation in deep brain regions (shown in warmer colours) are linked to shorter survival (time from brain scan to death), as illustrated by the downward trend between subcortical inflammation and survival time in the plot.
What is the impact?
Overall, the results suggest that MRI measures of deep brain shrinkage, inflammation PET scans, and blood NfL tests can help doctors and researchers better estimate prognosis in PSP and design more efficient treatment trials.
In addition, these findings add evidence to the role of inflammation in the brain in PSP and its association with clinical progression, thus supporting testing anti-inflammatory or immune-based therapies as possible disease‑modifying treatments for PSP.
One of the biggest challenges in PSP research is identifying markers that reliably track disease progression. By linking brain shrinkage, inflammation and blood markers to survival, our study highlights tools that could improve prognosis and make clinical trials more efficient.
Emerging Leader
Reference: Noah L Shapiro, Peter Simon Jones, Elijah Mak, Kamen A Tsvetanov, Julia Goddard, Davi S Vontobel, Robert Durcan, Leonidas Chouliaras, Tim Fryer, Young T Hong, Franklin Aigbirhio, Amanda Heslegrave, Nicolai Franzmeier, Matthias Brendel, Henrik Zetterberg, John T O’Brien, James B Rowe, Maura Malpetti, Inflammation PET and plasma neurofilament light predict survival in people with progressive supranuclear palsy, Brain Communications, Volume 7, Issue 6, 2025, fcaf467, https://doi.org/10.1093/braincomms/fcaf467